Recently, Professor Wu Meng from Washington University in St. Louis, USA, and Professor Dennis L. Kasper from Harvard Medical School, have unveiled the mystery of the intestinal complement system.
For a long time, the scientific community has widely believed that the complement system is merely an innate immune component in the blood, playing a key role in the body's immune defense. Professor Wu Meng and his collaborators discovered an independent complement system within the intestine.
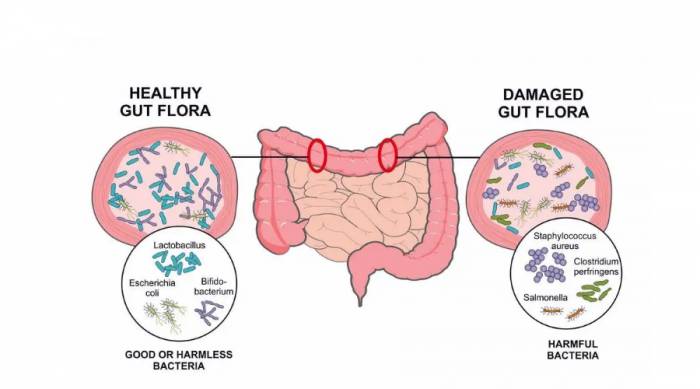
By selectively expressing specific complement components, under the regulation of the intestinal symbiotic microflora, this system can coexist harmoniously with the symbiotic microbial system and effectively eliminate pathogens.
Previous studies have found that an increased level of C3 in the intestine is a symptom of patients with inflammatory bowel disease and Crohn's disease. However, the intestinal expression of C3 and its role in the disease are not yet clear.
Advertisement
In the latest research, Professor Wu Meng and his team have, for the first time, discovered direct evidence of the complement component 3 (C3) in the intestine, revealing that intestinal microbes can regulate the level of C3 in the intestine and the protective role of intestinal C3 in resisting intestinal infections.Additionally, this research team has, for the first time, revealed that C3 is not only produced by liver cells, but it can also be produced by cells of the intestine and secreted into the intestinal lumen.
The study indicates that the complement system plays a more complex and comprehensive role in the body's defense mechanisms, particularly in maintaining a healthy balance of microbiota, with specific bacteria and bacterial products being able to regulate the expression of C3.
The research team further explored how the C3 components on the mucosa exert their effects, their cellular origins, and the dependency of these expressions on the host microbiota, thereby expanding our understanding of the production and function of the complement protein C3.
In summary, this work has opened up new directions for the study of the complement part of the immune system. It can also provide new preventive and therapeutic ideas for treating intestinal infections, inflammatory bowel disease, and Crohn's disease by regulating the interaction between the intestinal flora and intestinal complement.The "Ancient" Complement System and Gut Microbiota
As an ancient host defense mechanism, the complement system is composed of a series of proteins and is an essential part of the innate immune system.
The "ancient" nature of the complement system is reflected in two aspects:
On one hand, the complement system is particularly ancient in terms of biological evolution. Its biological origins can be traced back more than a billion years, and it already existed in coelenterates and protostomes. This evolutionary conservatism indicates its crucial function within organisms.
On the other hand, the complement system is one of the earliest biological systems that humans have studied in depth. At the end of the 19th century, the Belgian immunologist and microbiologist Jules Bordet discovered the presence of the complement system in the blood, for which he was awarded the Nobel Prize in Physiology or Medicine in 1919.In the century that followed, scientists gradually discovered more components of the complement system, among which the complement protein C3 is considered its core protein, related to both upstream and downstream pathways. For a long time, it was believed that C3 was mainly produced by hepatocytes, and the complement system mainly functioned in blood and interstitial fluid.
In recent years, with the advancement of modern sequencing technology, people have gained a deeper understanding of the gut microbiota. The academic community has found that the human gut has a rich microbial community, including bacteria, archaea, fungi, protozoa, and viruses.
These microorganisms can coexist harmoniously with humans and have an important impact on human health. At the same time, scientists have also revealed the complex and subtle relationship between the gut flora and the immune system.
Among them, the gut flora not only has the function of training the immune system, but the immune system can also regulate the gut flora to a certain extent.
However, in the gut, this environment rich in microorganisms, does the complement system exist? If it does, how does it interact with the symbiotic microbial community and pathogens? To answer such an ancient and modern question, the research team carried out this study.The Ingenious Human Intestinal Complement System
After setting the research direction, they carried out a series of studies centered on C3.
Firstly, the research team used germ-free mouse models and microbiome analysis to demonstrate that the gut microbiota can indeed regulate the levels of the complement protein C3.
Through this, they identified and isolated a bacterial strain that could specifically increase the level of intestinal complement protein C3. They also verified its effect in animal models.Further, they found that the levels of C3 in the blood were less influenced by the gut microbiota. Thus, they inferred that C3 should be produced by some kind of cell within the gut, which is produced in response to signals from the gut microbiota.
Therefore, the research team began to search for the study of this kind of gut cell. By combining single-cell RNA sequencing, flow cytometry analysis, in situ staining, and a series of other experimental methods, they found that the stromal cells in the intestinal lymphoid follicles are the richest source of C3 under steady-state conditions.
Although intestinal epithelial cells and immune cells can also produce C3 to some extent, this is the first time that intestinal stromal cells have been found to express C3.
As a result, they established an in vitro culture system, proving that intestinal stromal cells can directly sense symbiotic signals, then express C3 and secrete it outside the cell.
To determine the function of the intestinal complement system, they conducted new experiments and found that during infection, the level of C3 produced by the gut will increase, and all three types of cells will be involved in the protection against invasive pathogens.Then, C3 exerts its function through the alternative complement pathway, and bacteria marked by C3 are phagocytosed by neutrophils.
Furthermore, the baseline level of intestinal C3 determined by a healthy gut microbiota is inversely correlated with the severity of infection.
Finally, after testing and analyzing human intestinal samples, they confirmed that the intestinal complement system also exists in humans and is regulated by the gut microbiota.
After confirming the presence of complement protein C3 in the intestine, they faced such a question:
On the one hand, this experiment clearly demonstrates that there is a considerable amount of complement protein C3 in healthy mice and humans carrying gut microbiota;
On the other hand, traditional immunological research has shown that C3 is a protein with bactericidal properties, which "kills bacteria on sight" in the bloodstream.
However, due to the abundance of bacteria in the gut, they couldn't help but wonder how C3 coexists peacefully with these bacteria.
To this end, they attempted to track the behavior of C3 in a healthy gut using various methods, but they have not been able to find a clear answer. It was not until they studied the invasion of pathogens into the gut that they made some progress.
They found that under these circumstances, C3 mainly plays a role through phagocytic cells such as neutrophils. And in the gut, there is no pore-forming protein (C5-C9).
With this, the question became clear. In a healthy gut, there are relatively fewer neutrophils, even if some probiotics are marked by C3.However, due to the two downstream pathways of C3, namely the formation of the membrane attack complex on the bacterial membrane and the phagocytic cells that can engulf and digest microorganisms, such as neutrophils, both of which are present in very low quantities in a healthy gut, the gut complement can coexist peacefully with probiotics.
"When we discovered this phenomenon, we were amazed by the ingenious design of the human gut complement system. It is a very smart system that achieves precise regulation of probiotics and harmful bacteria by selectively expressing different molecules."
The gut complement system is like a guard within the human gut. They are responsible for patrolling and can coexist peacefully with probiotics. Once harmful bacteria appear, they can quickly and effectively eliminate them," said Wu Meng.
Eventually, the related paper was published in the journal Cell with the title "Gut complement induced by the microbiota combats pathogens and spares commensals" [1], with Wu Meng and Zheng Wen as the first authors, and Harvard Medical School Professor Dennis L. Kasper as the corresponding author.
Currently, the Washington University in St. Louis, where Wu Meng is located, is the earliest place where gut microbiota research began.She stated, "Our school's sequencing center was once one of the top three sequencing centers in the United States, having undertaken the Human Genome Project.
In such an academic environment, my research group employs a variety of research methods to study germ-free mouse models and human samples, dedicated to exploring the molecular regulatory mechanisms of the gut microbiota on the host."
Through this study, they found that the intestinal complement system is a new and promising direction for research.
There are many issues worth further exploration in the future: How does the gut microbiota regulate the levels of complement protein C3? Is it through metabolic products produced by bacteria, or through some structural molecules on the surface of bacteria? What are the receptors on the host cells?
It is expected that by delving deeper into the interactions between the gut microbiota and the complement system, new avenues will be opened for precision medicine targeting microbes, thereby achieving the prevention and treatment of intestinal diseases.
Comments